Study finds evidence of persistent Lyme infection in brain despite aggressive antibiotic therapy
Tulane University researchers found the bacterium that causes Lyme disease in the brain tissue of a woman who had long suffered neurocognitive impairment after her diagnosis and treatment for the tick-borne disease. The presence of the corkscrew-shaped Borrelia burgdorferi spirochetes in the former Lyme disease patient’s brain and spinal cord were evidence of a persistent infection.
The findings were published in Frontiers in Neurology.
The 69-year-old woman, who experienced progressively debilitating neurological symptoms throughout her illness, decided to donate her brain to Columbia University for the study of the disease as her condition worsened. While she had first experienced the classic symptoms of Lyme disease 15 years prior and was treated accordingly after her diagnosis, she experienced continual neurological decline including a severe movement disorder and personality changes, and eventually succumbed to Lewy body dementia. Lewy body dementia is associated with abnormal protein deposits in the nerve cells of the brain which can cause impairment in thinking, movement and mood, leading to a severe form of dementia.
“These findings underscore how persistent these spirochetes can be in spite of multiple rounds of antibiotics targeting them,”
Monica Embers
This is the first time researchers have identified a possible correlation between Lyme disease infection and Lewy body dementia.
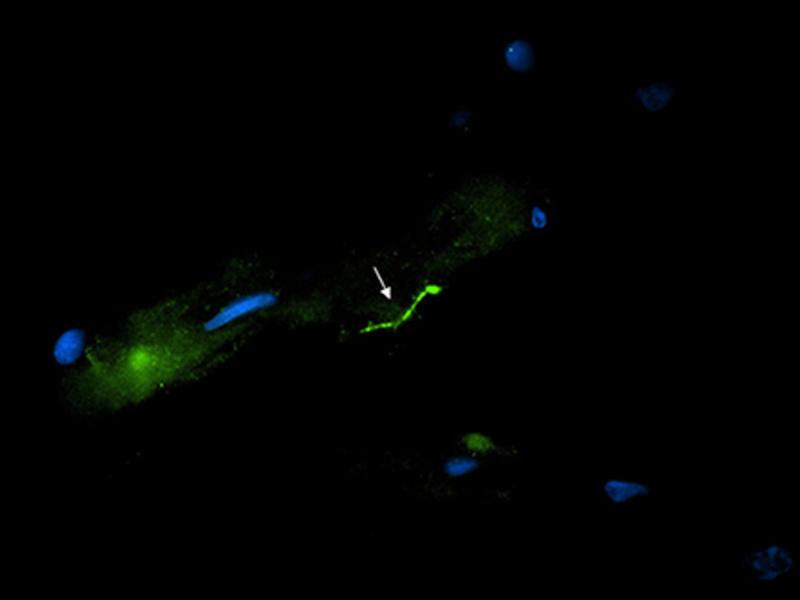
Using three highly sensitive methods of detection validated with nonhuman primate samples at Tulane National Primate Research Center, the research team concluded that at the donor’s time of death, her central nervous system (CNS) still harbored intact spirochetes in spite of aggressive antibiotic therapy for Lyme disease at different times throughout her illness. They employed the use of immunofluorescence staining to image the spirochetes, polymerase chain reaction or PCR to detect the presence of B. burgdorferi DNA, and RNAscope to determine whether the spirochetes were viable.
Previous research by the lead author of the study, Monica Embers, associate professor of microbiology and immunology at Tulane, concluded that a B. burgdorferi infection could persist in the CNS of rhesus macaques following the standard course of doxycycline prescribed for Lyme disease. Embers hopes that these latest findings help pave the way for investigating the presence of B. burgdorferi in the autopsies of other patients who have experienced severe neurocognitive decline.
“These findings underscore how persistent these spirochetes can be in spite of multiple rounds of antibiotics targeting them,” Embers said. “We will be interested in investigating the role that B. burgdorferi may play in severe neurological disease, as this is an area of research that has not yet been fully explored.”
About 15% of patients diagnosed with Lyme disease experience neuroborreliosis, a systemic infection of spirochetes which can affect both the CNS and peripheral nervous system.
This study was done in collaboration with Dr. Brian Fallon of the Lyme and Tick-Borne Diseases Research Center at Columbia University Irving Medical Center.