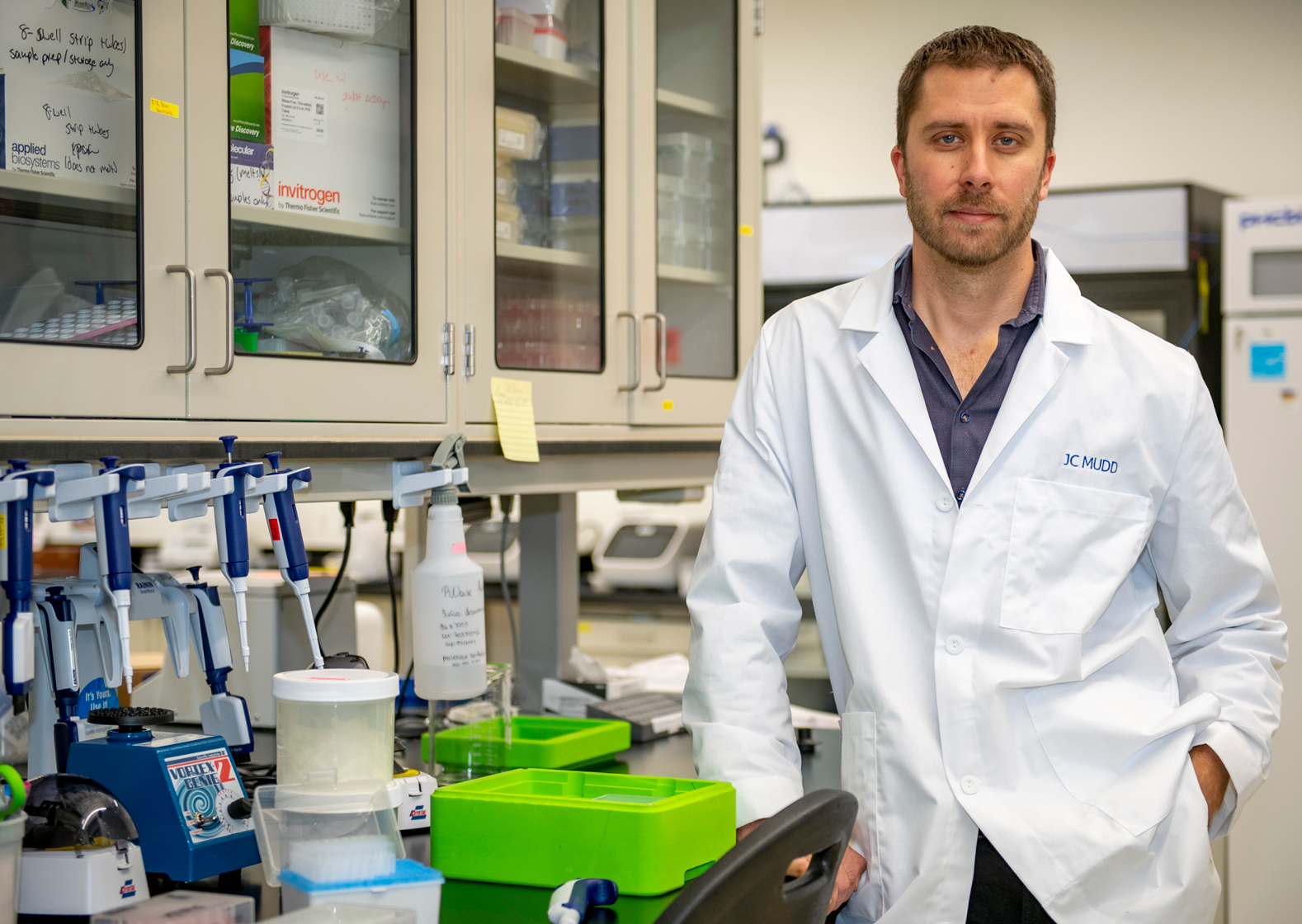
Joseph Mudd, PhD
Assistant Professor of Microbiology and Immunology
Education & Affiliations
Research
HIV-1 can persist in latent form where the virus integrates its genetic material into the host genome and becomes virtually invisible to host-immune recognition. The persistence of CD4 T cells harboring latent HIV-1 (deemed ‘reservoir’) is the principle reason why HIV-1 infection is incurable and remains a continual public health burden. Because latent HIV-1 is silent and undergoes little to no transcription, latent-infected cells behave in very similar ways to uninfected cells and it is very difficult to target them. Our lab employs both cell-based and sequencing approaches in the NHP model to study how immune responses to a common co-infecting virus CMV contribute to maintaining the reservoir. The lab also explores the role of diet and how nutritional interventions can influence SIV pathogenesis and persistence
